All (Adult) Vaginas Need Estrogen

The Sexual Health Double Standard and (Exactly) How to Fix It
Each year, the world spends $3 billion on Viagra and other PDE5i medications because, as a society, we've acknowledged that men's sexual health matters. It's important for relationships and pleasure, yes, but also for their mental and emotional health. Because it's valued, men happily invest in these medications, and doctors readily prescribe them.
Now imagine saying this to a man going through menopause:
"Okay, Mr. Smith, here's what's going to happen. First, your penis is going to dry up - like Sahara desert dry. We'll provide you with plenty of lubricant to keep on hand.
Next, the healthy bacteria around your penis will disappear, creating an environment that is ripe for infection. We'll treat those with antibiotics, which will destroy your gut flora and cause other problems, but don’t worry, it's fine.
Then your pelvic floor muscles will weaken, so there's a good chance your internal organs will start falling out or you'll lose bladder control. Costco has great deals on adult diapers.
Finally, you'll not only notice less desire, sensation, and a harder time reaching climax, but you'll also see SHRINKING of your penis. It may become hard to find. I recommend your partner invest in a good magnifying glass."
Can you imagine? Yet this is essentially what we tell women about menopause, and then we act surprised when they're unhappy about it.
This is medical gaslighting at its finest, and it's time we called it out.
Low Dose Vaginal Estrogen to the Rescue?
Yes, we have a solution. Yes, we've known about it for decades. Why so few women and their doctors know about this elegant fix for low estrogen states affecting the pelvic floor remains a mystery.
In this article, I'm diving deep into low-dose vaginal estrogen as a safe, effective, and inexpensive solution for genitourinary syndrome of menopause (GSM) and other hypoestrogenic states - whether from breastfeeding, birth control pills, or overtraining - that wreak havoc on vaginal and vulvar health.
Unlike systemic estrogen (patches, gels, pills, etc.), low-dose vaginal estrogen stays local, targeting the pelvic floor where it is needed most, with minimal systemic absorption.
Hold onto your hats—this is the Who, What, Where, Why, and Exactly How of low-dose vaginal estrogen for sexual and pelvic floor health. Giddy up!
The Estrogen-Viagra Connection: More Similar Than You Think
Before we get into the “how,” let’s talk about one of the big “whys”: better sexual health. I hear women complain about not having a “Viagra for women,” but really, estrogen IS exactly that.
Estrogen and Viagra are remarkably similar in how they support sexual health. Both provide immediate functional benefits while also promoting long-term tissue health.
Let’s break it down.
Viagra's Dual Action in Men:
- Immediate: Prevents breakdown of cGMP, allowing nitric oxide to work longer and maintain blood flow.
- Long-term: Improves endothelial function (the cells that line blood vessels) and maintains healthy smooth muscle cells (within the penis).
- Systemic benefits: When used systemically, PDE5 inhibitors like Viagra show potential for heart and brain protection.

Estrogen's Dual Action in Women:
- Immediate: Increases nitric oxide production and improves blood flow to pelvic tissues.
- Long-term: Rebuilds collagen and elastin, promotes new blood vessel growth, maintains muscle tone and strength.
- Systemic benefits: When used systemically, it may protect the brain and cardiovascular system.
The Key Similarity: Both medications work through the nitric oxide pathway to improve blood flow immediately, while simultaneously supporting the long-term health of the tissues they're targeting. And both show promise for broader health benefits when used systemically.
This Substack is reader-supported. To read the rest of this article and support my work, consider becoming a paid subscriber.
The Science Behind Estrogen's Magic
The entire urogenital tract is essentially an estrogen-dependent ecosystem. Estrogen receptors (ERα, ERβ, and GPER) are found throughout the vaginal epithelium, urethra, bladder, pelvic floor muscles, and supporting connective tissues. This isn't coincidental; it's evolutionary design.
Here's what estrogen does for your pelvic floor:
1. Structural Support
Estrogen increases collagen I and III synthesis while suppressing the enzymes (matrix metalloproteinases) that break down collagen. Translation: it literally rebuilds the scaffolding that holds everything together. When estrogen drops, this scaffolding starts collapsing, leading to pelvic organ prolapse and tissue weakness.
2. Infection Protection
Estrogen helps maintain the vaginal microbiome by supporting beneficial lactobacillus bacteria, which keep the pH in the healthy range (3.8-4.5). This acidic environment prevents harmful bacteria and yeast from establishing themselves. Lose estrogen, lose this protection, which is why UTIs and yeast infections skyrocket after menopause.
3. Vascular Health
Just like Viagra improves blood flow to penile tissue, estrogen maintains optimal blood flow to vaginal and vulvar tissues. This ensures adequate oxygen and nutrients reach the area for maintenance and repair.
4. Neural Function
Estrogen helps regulate the density and sensitivity of the nerves in the female genital tract. You know what has a hell of a lot of estrogen and blood-flow-loving nerve endings (10,281 to be precise): Your clitoris! No wonder the “Big O” becomes more elusive after estrogen drops!
The Clinical Evidence
Here's how well low dose vaginal estrogen works:
- Reduces recurring UTI risk by 36-75% (decreasing the risk of sepsis by half and mortality from UTIs by 73%!)
- Supports bladder function and pelvic floor muscles, reducing urinary incontinence by 24%.
- Improves all sexual domains: libido, arousal, lubrication, orgasm, satisfaction, and pain reduction.
Safety Profile:
Even in breast cancer survivors, historically the most cautious population for estrogen therapy, a 2024 systematic review of over 60,000 women found that vaginal estrogen did NOT increase:
- Breast cancer recurrence
- Breast cancer mortality
- Overall mortality rates
In fact, some studies suggest a protective effect.
Who Needs Vaginal Estrogen? (Spoiler: Probably You)
Menopausal Women
If you're in menopause (or even perimenopause) and are experiencing any changes in vaginal comfort, lubrication, or urinary function, you're a candidate. The 2025 AUA guidelines now recommend low-dose vaginal estrogen as first-line therapy for moderate to severe genitourinary syndrome of menopause (GSM).
Here's a crucial point few doctors talk about: even if you're taking systemic oral or transdermal estrogen for hot flashes (etc), up to 25% of you will still experience vaginal symptoms. Systemic estrogen helps, but it often isn't enough for complete GSM relief. Adding vaginal estrogen to your regimen is not only safe, but current guidelines recommend it. Yay!
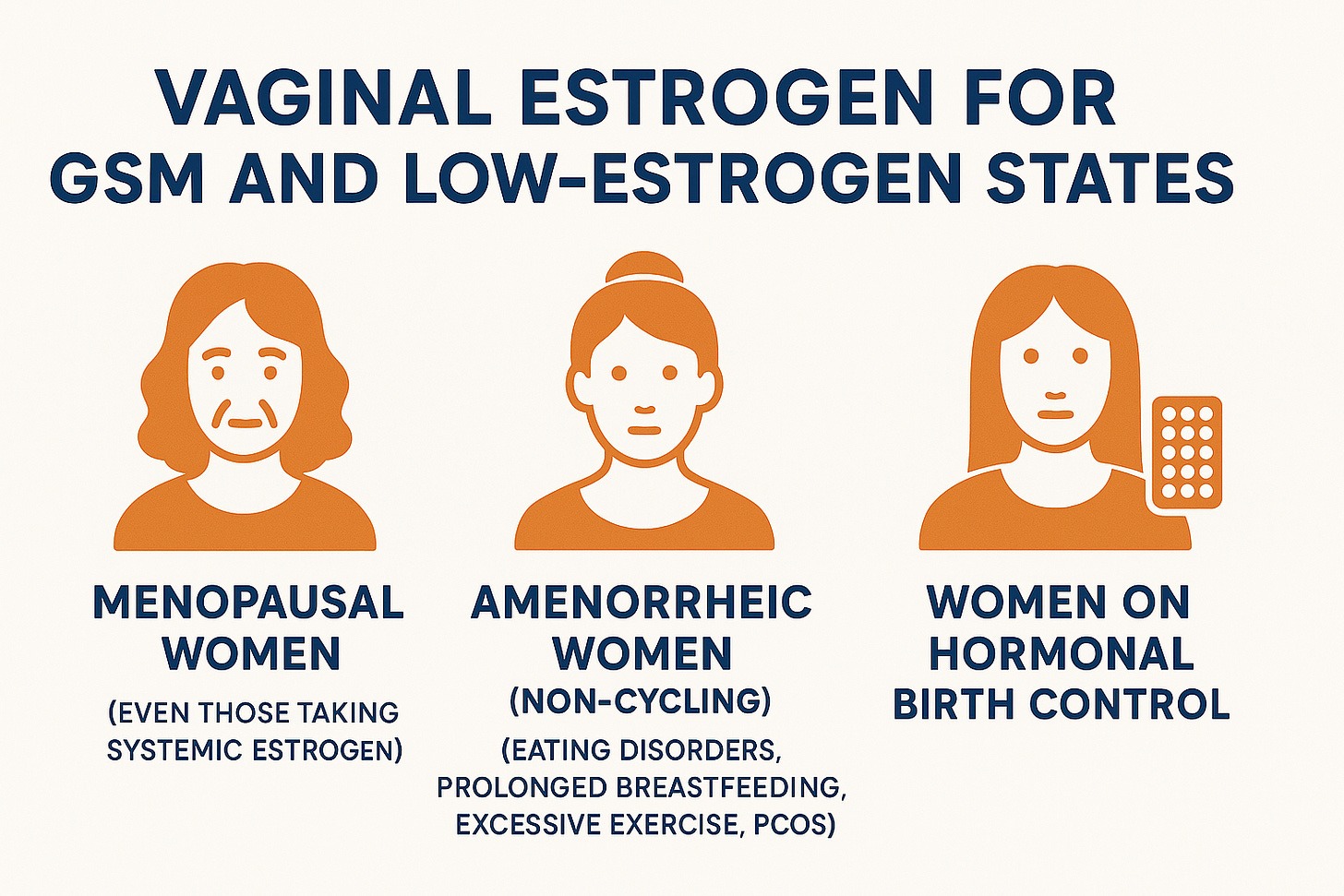
Amenorrheic Women (Non-Cycling)
This is the group we often forget about. Women experiencing amenorrhea (lack of menstrual cycles) from breastfeeding, eating disorders, excessive exercise, or PCOS can develop the same estrogen-deficiency changes as menopausal women, often in their 20s and 30s. These women deserve the same treatment options.
Women on Hormonal Birth Control
About 15% of women taking hormonal birth control experience GSM-like symptoms due to low estrogen states. The biggest offenders are the progestin-only forms (mini-pill or depo shots) and the low-dose combined oral contraceptives. Higher-dose combined oral contraceptives and IUDs are less likely to cause GSM symptoms (although any oral birth control will reduce your free testosterone, which may contribute to sexual dysfunction).
Practical Application: Getting What You Need
The Gold Standard Dose
The most commonly prescribed and studied formulation is estradiol 0.01% cream, 1 gram applied vaginally three times per week. This provides approximately 0.1 mg of estradiol per dose, a tiny amount that stays primarily localized to vaginal tissues. This is a prescription medication.
Alternative Hormone Options
Vaginal DHEA (Intrarosa):
- Dose: 6.5 mg inserted nightly at bedtime.
- Converted locally to both estradiol and testosterone.
- May provide superior improvement in overall sexual function.
Note: Julva is an over-the-counter vulvar moisturizer containing DHEA and several natural oils. It’s applied externally and is a good option if you can’t obtain a prescription for hormones or simply want additional moisturizing benefits. If you want to try it out, use “KILLENIT” for a discount*.
Estriol Options:
- Weaker estrogen (8% potency of estradiol) with an excellent safety profile.
- Available as creams or pessaries.
- Equally effective for vaginal symptoms (but requires a higher dose than estradiol)
“Just the Tips” That Matter
Forget what you think you know about vaginal application. Here's what works:
The Finger Method (Often Better Than Applicators):
- Use the applicator to measure the dose initially.
- Squeeze measured cream onto a clean finger.
- Apply directly to vaginal opening AND urethral area.
- Insert only about 1-2 inches. Deep insertion isn't necessary.
Strategic Placement:
- Add a small amount to external vulvar tissues as well (your clitoris says “thank you”!)
- Apply at bedtime to reduce leakage (and yes, expect some leakage).
What to Expect
- Effects begin within 2-3 weeks.
- Optimal results by 2-3 months (be patient!).
- Initial vaginal discharge is normal as tissues rehydrate.
- No routine monitoring required for low-dose preparations.
Pharmaceutical vs. Compounded
Pharmaceutical options:
- Estrace cream (estradiol)
- Vagifem tablets (estradiol)
- Estring ring (estradiol)
- Imvexxy inserts (estradiol)
- Intrarosa (DHEA)
Hot tip: You can get a tube of Estrace from Cost Plus Drugs in the U.S. for $13.21.

Compounded options: While not necessary for most women, these “made in-house” hormone formulations are an excellent option for the up to 25% of women who report burning, irritation, or increased discharge from using commercial vaginal estrogen creams.
Commercial products like Estrace and Premarin contain a combination of potential irritants, including propylene glycol, parabens, benzyl alcohol, artificial dyes, mineral oil, and sometimes sodium lauryl sulfate. For women who react to these additives, compounded estrogen can be a game-changer.
The Ellage Anhydrous Advantage: One of my favorite discoveries is the Ellage™ Anhydrous Vaginal Cream Base, specifically designed for sensitive vaginal tissues. This water-free base is:
- Free from common allergens (wheat, milk, egg, soy, fish, nuts, gluten).
- No artificial dyes, fragrances, parabens, or propylene glycol.
- pH-neutral and non-irritating to vaginal tissue.
- Known to reduce leakage by tightly adhering to the vaginal mucosal tissue.
When to consider compounded options:
- Sensitivity to commercial product ingredients
- Recurrent burning or irritation without infection
- Need for custom dosing or combination therapy
Your doctor can prescribe compounded estradiol, estriol or DHEA and specify allergen-minimizing bases through reputable compounding pharmacies.
Frequently Asked Questions:
Do I also need to take progesterone?
Short answer: No. Low-dose vaginal estrogen has minimal systemic absorption and doesn't stimulate the endometrium (uterine lining). Multiple professional guidelines (NAMS, ACOG, AUA) confirm progesterone is "generally not indicated" with low-dose vaginal estrogen.
Can I take both systemic AND vaginal estrogen?
Absolutely, and it often works better that way. The 2025 AUA guidelines explicitly state that for women on systemic estrogen who continue to have GSM symptoms, adding localized vaginal estrogen is recommended. The vaginal dose is so low that it doesn't significantly increase systemic exposure.
Will low dose vaginal estrogen improve my other menopause symptoms, such as hot flashes, mood changes, or heart palpitations?
No. It is a localized medication so only works in your pelvic floor.
Can I start it if I’m more than ten years out from menopause onset?
Yes. Absolutely. Start it at any age. Stay on it forever.
Can I take it if I’ve had blood clots, heart problems, strokes, migraines with aura, or breast cancer?
Yes. Despite the FDA’s absurd (black) boxed warning, low-dose vaginal estrogen is extremely safe. Remember, it doesn’t significantly increase the estrogen levels in your blood at the doses we’re talking about here. In July, 2025 an expert panel convened by the FDA strongly urged the agency to revise or remove this warning, citing current evidence that demonstrates the previous risk warnings are inaccurate for low dose vaginal estrogen.
Call Out: Great job to the physician panelists who spoke to the FDA on behalf of vaginal estrogen relabeling, better menopause education and patient advocacy…Kelly Casperson, MD, Heather Hirsch MD MS MSCP , Rachel Rubin , Dr Vonda Wright , JoAnn Pinkerton , Roberta Diaz Brinton . 💪
Can I take it in a car? Can I take it in a bar? Can I take it in my house? Near a mouse? Can I take it here or there? Can I take it anywhere?
Yes. But really, taking it before bed is easiest. :)

The Bottom Line: Your Vagina Deserves the Same Respect as His Penis
Every adult vagina - whether you're 25 with amenorrhea, 45 in perimenopause, or 75 and well past the menopause transition - deserves access to estrogen. If you don’t make it, take it.
If you're experiencing any changes in vaginal comfort, lubrication, sensation, or urinary function, vaginal estrogen should be part of the conversation with your doctor. It's one of the most effective, safest, least expensive interventions we have for maintaining sexual and urinary health. Print this article out and take it with you to your doctor’s office!
We wouldn't tell a man with erectile dysfunction to "just use more lube and hope that glass of wine kicks in soon," so why is this our default response to women's sexual health concerns?
I’m asking for a friend. And that friend is your vagina.
*Financial disclosure: I am an affiliate for Julva Vaginal Moisturizer, which means that I make a small commission if you order with my discount code. It’s not enough to buy me a truck (which I’ve recently decided I need) but maybe it’ll buy me a bumper sticker that says “All Vaginas Need Estrogen.” 😁
Have you noticed changes to your sexual or pelvic floor health? Has your doctor discussed low-dose vaginal estrogen or DHEA with you? I’d love to hear about your experiences! And, share this article with your mom, sister, daughter and DOCTOR!
About the Author: Dr. Amy B. Killen, M.D., is a leading physician in regenerative and hormone optimization medicine, specializing in women's health and helping patients navigate their "Queen Phase™" with evidence-based interventions. A board-certified emergency physician turned longevity specialist, she combines cutting-edge treatments, such as stem cell therapy, hormone optimization, and peptides, with practical lifestyle wisdom at her clinics in Utah, Texas, and Florida while sharing her expertise through international speaking engagements and educational content creation.
As Chief Medical Officer of Humanaut Health and founder of the Human Optimization Project (HOP), Dr. Killen is passionate about advancing women’s longevity medicine. Subscribe to her substack here.
References:
Primary Guidelines
2025 AUA/SUFU/AUGS GSM Guidelines
- Kaufman MR, Ackerman LA, Amin KA, et al. The AUA/SUFU/AUGS Guideline on Genitourinary Syndrome of Menopause. J Urol. 2025. doi:10.1097/JU.0000000000004589
- Link: https://www.auajournals.org/doi/10.1097/JU.0000000000004589
Major UTI Prevention Studies
Kaiser Permanente Large Cohort Study (5,638 women)
- Tan-Kim J, Shah NM, Do D, Menefee SA. Efficacy of vaginal estrogen for recurrent urinary tract infection prevention in hypoestrogenic women. Am J Obstet Gynecol. 2023 Aug;229(2):143.e1-143.e9. doi:10.1016/j.ajog.2023.05.002
- Link: https://pubmed.ncbi.nlm.nih.gov/37178856/
Epic Cosmos Database Study (11+ million patients)
- Wells BA, De E, et al. Impact of Vaginal Estrogen on Serious Adverse Outcomes in Postmenopausal Women with Recurrent UTI. Abstract presented at AUA 2025
- Link: https://www.ics.org/2025/abstract/118
Randomized Clinical Trial
- Ferrante KL, Wasenda EJ, Jung CE, Adams-Piper ER, Lukacz ES. Vaginal Estrogen for the Prevention of Recurrent Urinary Tract Infection in Postmenopausal Women: A Randomized Clinical Trial. Female Pelvic Med Reconstr Surg. 2021 Feb;27(2):112-117. doi:10.1097/SPV.0000000000000749
- Link: https://pubmed.ncbi.nlm.nih.gov/31232721/
Breast Cancer Survivor Safety Studies
Major Meta-Analysis
- Beste ME, Kaunitz AM, McKinney JA, Sanchez-Ramos L. Vaginal estrogen use in breast cancer survivors: a systematic review and meta-analysis of recurrence and mortality risks. Am J Obstet Gynecol. 2025 Mar;232(3):262-270.e1. doi:10.1016/j.ajog.2024.10.054
- Link: https://pubmed.ncbi.nlm.nih.gov/39521301/
Large Population Study
- McVicker L, Labeit AM, Coupland CAC, et al. Vaginal Estrogen Therapy Use and Survival in Females With Breast Cancer. JAMA Oncol. 2024;10(1):103–108. doi:10.1001/jamaoncol.2023.4508
- Link: https://jamanetwork.com/journals/jamaoncology/fullarticle/2811413
Alternative Hormone Studies
DHEA Clinical Trials
- Labrie F, Archer DF, Koltun W, et al. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2018 Nov;25(11):1339-1353. doi:10.1097/GME.0000000000001238
- Link: https://pubmed.ncbi.nlm.nih.gov/30358731/
- Labrie F, Archer DF, Bouchard C, et al. Intravaginal dehydroepiandrosterone (prasterone), a highly efficient treatment of dyspareunia. Climacteric. 2011 Apr;14(2):282-8. doi:10.3109/13697137.2010.535226
- Link: https://pubmed.ncbi.nlm.nih.gov/21244215/
AHRQ Evidence Report
- Danan ER, Diem S, Sowerby C, et al. Genitourinary Syndrome of Menopause: A Systematic Review and Meta-analysis of Treatment Effectiveness. AHRQ Publication No. 24-EHC022. Agency for Healthcare Research and Quality. July 2024
- Link: https://effectivehealthcare.ahrq.gov/sites/default/files/related_files/cer-272-genitourinary-syndrome-executive-summary.pdf